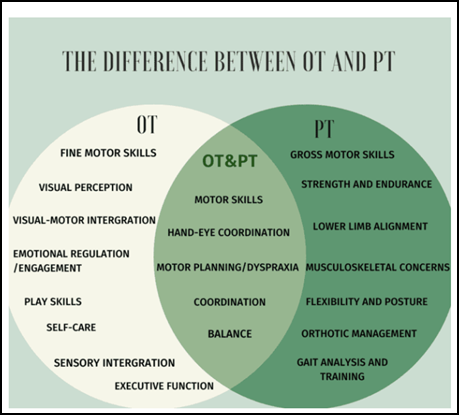
Autumn brings a unique blend of colors, textures, and sensory experiences that make it an ideal season for therapeutic play. For children participating in occupational therapy (OT), the fall months offer numerous opportunities to develop essential life skills through creative, hands-on activities. The crisp air, earthy scents, and natural materials invite exploration and engagement, powerful motivators for children working on fine and gross motor skills, coordination, and sensory integration.
Home-based occupational therapy activities allow children to practice skills in comfortable, familiar environments, often leading to greater confidence and participation. Seasonal themes, such as pumpkins, leaves, and apples, can make therapeutic exercises feel more like play than structured therapy sessions. By aligning activities with a child’s interests and the natural rhythms of the season, parents can reinforce developmental progress while nurturing creativity and curiosity.
Crafting and sensory play are at the heart of this approach. These activities combine fun with functional goals, strengthening fine motor control, promoting bilateral coordination, and supporting self-regulation. Whether it’s squeezing glue onto a pumpkin seed mosaic or raking leaves into a pile, every movement can serve a purpose in building a child’s physical and cognitive foundation.
Sensory-Rich Autumn Crafts for Fine Motor Skills

Fall crafts are powerful tools for enhancing hand strength, dexterity, and sensory awareness. Engaging a child’s tactile senses and creativity helps improve their ability to manipulate small objects, which is vital for daily activities like writing, buttoning, and tying their shoes.
Below are several autumn-themed crafts that combine sensory exploration with developmental goals:
- Leaf Rubbing Art:
Collect fallen leaves, place them under a sheet of paper, and rub crayons or colored pencils over the surface. This activity encourages hand strength and coordination while allowing children to explore different textures. The sensory feedback from the uneven leaf surface helps refine tactile discrimination, a core element of sensory processing. - Pumpkin Seed Mosaics:
After cleaning and drying pumpkin seeds, use them to create seasonal mosaics on cardboard or paper plates. Picking up and placing each seed strengthens the pincer grasp and promotes bilateral coordination. Painting or dyeing the seeds adds a creative element that enhances visual-motor integration. - Apple Stamping:
Cut an apple in half, dip it in washable paint, and stamp patterns on paper. This fun, messy craft builds grip strength and introduces children to cause-and-effect play. Encouraging them to press down with even pressure supports fine motor control and sensory regulation. - Textured Autumn Collages:
Use natural and craft materials, like burlap, cotton balls, dried leaves, and fabric scraps, to create tactile collages. Children can cut, glue, and layer items to stimulate multiple senses. The varied textures encourage exploration while supporting bilateral hand use and visual scanning.
By incorporating sensory-rich materials into these crafts, parents can reinforce fine motor skills while helping children build confidence and independence through creative expression.
Gross Motor Activities Inspired by Fall

Gross motor play during autumn is equally beneficial for children in occupational therapy. These activities engage large muscle groups, improve balance and coordination, and help regulate sensory systems through active movement. Outdoor spaces filled with leaves, acorns, and crisp air become natural therapy rooms where movement feels joyful rather than clinical.
Here are some fall-inspired gross motor activities perfect for at-home therapy sessions:
- Scavenger Hunts for Leaves, Acorns, or Pinecones:
Create a list of fall items to find in the yard or park. As children bend, reach, and walk, they practice balance, body awareness, and motor planning. This kind of exploratory play also supports executive functioning and problem-solving. - Autumn-Themed Obstacle Courses:
Use everyday objects, like hay bales, boxes, and blankets, to design a fall-inspired obstacle course. Include activities such as jumping over “leaf piles,” crawling under “pumpkin tunnels,” and climbing “apple trees.” This type of play develops strength, bilateral coordination, and endurance while promoting spatial awareness. - Outdoor Nature Walks:
A simple walk in a local park can become a sensory adventure. Encourage children to notice sounds (crunching leaves), textures (bark or moss), and scents (earthy soil or pine). Walking on uneven terrain improves balance and coordination, while the calming environment can support self-regulation and attention. - Raking Leaves and Jumping in Piles:
What may seem like playtime is actually therapeutic exercise. Raking strengthens the arms, shoulders, and core, while jumping builds leg power and provides deep proprioceptive input, important for body awareness and emotional regulation.
Gross motor play in the fall gives children the chance to move freely and engage their senses in natural surroundings, helping them translate physical skills into functional daily activities.
Tips for Integrating Therapeutic Goals into Daily Autumn Routines

The beauty of home-based occupational therapy lies in its flexibility. Parents can seamlessly weave therapeutic objectives into everyday routines, ensuring consistent practice without making it feel like work. Seasonal activities, baking, decorating, or exploring nature, can all be adapted to support a child’s developmental needs.
Here are some practical ways to bring therapy into family life:
- Adapt Activities for Different Ability Levels:
Modify the difficulty of each task to meet your child’s current abilities. For example, younger children might sort leaves by color, while older children can trace and cut them out. This approach maintains engagement and promotes gradual skill-building. - Turn Everyday Fall Tasks into Therapy:
Baking seasonal treats, such as pumpkin muffins or apple crisp, offers opportunities to measure, stir, and pour, activities that strengthen bilateral coordination and sequencing skills. Decorating the home for fall can involve cutting shapes, tying ribbons, or hanging garlands, all beneficial for fine motor development. - Celebrate Progress through Playful Engagement:
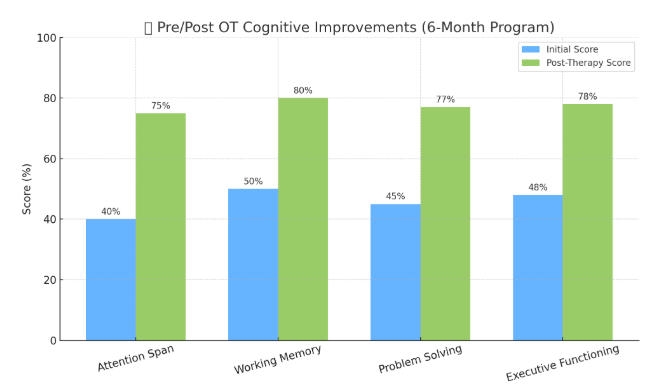
Recognizing small victories helps build motivation and self-esteem. Parents can track progress through photos or short notes after each activity, reinforcing the connection between play and growth. Even modest improvements in attention span or grip strength deserve acknowledgment. - Encourage Creativity and Flexibility:
Occupational therapy at home doesn’t have to follow strict guidelines. Allowing children to choose materials, adapt instructions, or create their own versions of activities fosters independence and self-expression. A flexible, child-led approach ensures therapy remains fun, empowering, and deeply meaningful.
Integrating therapeutic goals into family life ensures that progress doesn’t pause between clinical sessions. It transforms ordinary moments, baking, walking, and crafting, into rich opportunities for learning and connection.
The Power of Activities for Kids in the Autumn Season

Autumn’s sights, sounds, and textures offer a perfect backdrop for meaningful therapeutic experiences. By combining sensory play, creative expression, and physical movement, parents can help children meet occupational therapy goals while enjoying the season’s natural beauty. Each activity, from a simple leaf rubbing to an energetic nature walk, strengthens not only physical skills but also emotional resilience and confidence.
Home-based occupational therapy thrives when it’s grounded in joy and curiosity. Fall’s abundance of natural materials and playful themes makes it easier than ever to create enriching, goal-oriented experiences. Through creativity and consistency, families can turn everyday moments into stepping stones toward independence and growth, all while savoring the best that the season has to offer.
If you’re ready to make this fall a season of growth and creativity for your child, Tip of the Tongue Rehab can help. Our pediatric occupational therapists specialize in turning play into progress, whether through sensory-rich activities, fine motor development, or confidence-building routines.
Visit our Contact Page to schedule a consultation or learn more about our personalized home-based therapy plans. Let’s work together to help your child thrive this autumn and beyond.